Mission in Motion Fiscal Q1 Highlights
The Academy is proud to highlight the achievements of the first fiscal quarter with milestones that that moved the Academy and the profession forward with purpose and momentum.
Learn moreStay up to date on important happenings for nutrition and dietetics practitioners and students.
The Academy is proud to highlight the achievements of the first fiscal quarter with milestones that that moved the Academy and the profession forward with purpose and momentum.
Learn moreDeanne Brandstetter, MBA, RD, CDN, FAND, the Academy's 2025-26 President, shares important upcoming goals and changes for our organization.
Learn moreAcademy leadership discussed how our five-year strategic plan will drive progress and innovation. Members also gained timely insights on policy priorities and advocacy efforts, explored new research highlights and other key initiatives across the Academy.
Learn moreDeanne Brandstetter, MBA, RD, CDN, FAND, the Academy's 2025-26 President, shares important upcoming goals and changes for our organization.
Learn moreDeanne Brandstetter, MBA, RD, CDN, FAND, the Academy's 2025-26 President, shares important upcoming goals and changes for our organization.
Learn moreThe Academy has identified four focus areas where Food as Medicine programs promote health and prevent disease.
Learn moreExplore the Academy's achievements for fiscal year 2024-2025 as we celebrate our key successes.
Learn moreDeanne Brandstetter, MBA, RD, CDN, FAND, the Academy's 2025-26 President, shares important upcoming goals and changes for our organization.
Learn more
The following individuals have been selected in recognition of outstanding service and contributions to the nutrition and dietetics profession.
Learn moreHarlivleen "Livleen" Gill, MBA, RDN, LDN, FAND, the Academy's 2024-25 President, shares important upcoming goals and changes for our organization.
Learn moreHHS Secretary Kennedy and FDA Commissioner held a joint press conference to announce FDAs intent to phase out the use of petroleum based synthetic food dyes through actions and industry commitments.
Learn moreTo inform and support the development of the Academy's new strategic plan, a Current State Assessment was conducted to assess the existing landscape of the organization and profession and guide actionable strategies and priorities for the Academy moving forward.
Learn moreIn October 2024, through global research consultant Avenue M Group, the Academy conducted focus groups with members and nonmembers to explore the challenges, goals and value received from the Academy and alternative resources. Learn more, including how these insights will be used moving forward.
Learn moreHarlivleen "Livleen" Gill, MBA, RDN, LDN, FAND, the Academy's 2024-25 President, shares important upcoming goals and changes for our organization.
Learn moreThe Academy's work in inclusion, diversity, equity and access focuses on cultivating organizational and professional values of equity, respect, civility and anti-discrimination and expanding a culture of welcoming throughout the nutrition and dietetics community.
Learn moreIn 2020, the Academy commissioned The Exeter Group to conduct an analysis aimed at understanding members' perceptions, experiences and feedback on diversity, equity and inclusion.
Learn moreVarious focus groups and discussions were conducted at the 2024 Food & Nutrition Conference & Expo®. The feedback highlights both the need for and challenges in advancing Inclusion, Diversity, Equity, and Access (IDEA) within the Academy, as well as potential opportunities for improvement and future aspirations.
Learn moreWatch this message from Academy CEO Wylecia Wiggs Harris, PhD, CAE, to learn about the Academy’s mission to support and elevate the profession of RDNs and NDTRs, including what the Academy is doing now and in the near future.
Learn moreHarlivleen "Livleen" Gill, MBA, RDN, LDN, FAND, the Academy's 2024-25 President, shares important upcoming goals and changes for our organization.
Learn moreIn 2024, Blue Cross Blue Shield agreed to a $2.8 billion antitrust settlement, which includes substantial reforms affecting how BCBS-affiliated plans operate, with major implications for health care providers, employer-sponsored health insurance and consumer choice.
Learn moreHarlivleen "Livleen" Gill, MBA, RDN, LDN, FAND, the Academy's 2024-25 President, shares important upcoming goals and changes for our organization.
Learn moreThe Academy and its Foundation send our thoughts to those affected and offers a list of resources for wildfire recovery.
Learn moreHarlivleen "Livleen" Gill, MBA, RDN, LDN, FAND, the Academy's 2024-25 President, shares important upcoming goals and changes for our organization.
Learn moreHarlivleen "Livleen" Gill, MBA, RDN, LDN, FAND, the Academy's 2024-25 President, shares important upcoming goals and changes for our organization.
Learn moreThe approved 2024 ICD-10-CM codes went into effect on October 1, 2024, and will be in use until September 30, 2025. This update includes 395 new diagnosis codes, 25 deletions, and 13 revisions, with several changes relevant to registered dietitian nutritionists. Learn more about the new codes and how to use them.
Learn moreThe Academy’s National Honors and Awards recognize those who have advanced the profession, exhibited leadership and shown devotion to serving others. To prepare for upcoming deadlines, compile key documents in advance with these tips.
Learn moreThe Academy and its IDEA Committee will focus on these objectives over the next three years. Learn more about how the Academy will create a more inclusive and equitable organization that reflects the shared values of its community.
Learn moreHarlivleen "Livleen" Gill, MBA, RDN, LDN, FAND, the Academy's 2024-25 President, shares important upcoming goals and changes for our organization.
Learn moreHarlivleen "Livleen" Gill, MBA, RDN, LDN, FAND, the Academy's 2024-25 President, shares important upcoming goals and changes for our organization.
Learn moreHarlivleen "Livleen" Gill, MBA, RDN, LDN, FAND, the Academy's 2024-25 President, shares important upcoming goals and changes for our organization.
Learn more
The following individuals have been selected in recognition of outstanding service and contributions to the nutrition and dietetics profession.
Learn moreThe Academy's president's message to members concerning an article published in The Washington Post and The Examination regarding "anti-diet" advice and dietitians role in pushing that advice.
Learn moreIn alignment with our commitment to accessibility, sustainability and meeting the evolving needs of our readers, the Journal of the Academy of Nutrition and Dietetics (JAND) will transition to a digital-only format starting January 1, 2026.
Learn more
The Academy of Nutrition and Dietetics received the Gold MyPlate Champion achievement for its participation in the MyPlate National Strategic Partnership and for efforts promoting MyPlate for the inaugural cycle of Partner Recognition Program.
Learn moreFor the first time in its history, the Academy of Nutrition and Dietetics has released policy statements and evidence-informed rationales for each of the organization's focus areas. The statements and supporting rationale outlined in the President’s Strategic Advancement Groups Report will be instrumental in shaping the Academy’s future policy and advocacy efforts.
Learn more
The Academy remains committed to improving the nation’s health and advocating for policies that support the five pillars in the National Strategy, with Academy members playing a key role.
Learn moreA news article written by a reporter who has targeted registered dietitian nutritionists before is expected to appear in the coming days and could be critical of some RDNs and the Academy. Academy President Lauri Wright conducted an interview with the reporters and provided facts and statistics in writing to ensure accuracy.
Learn more
The ending of the public health emergency in May 2023 has continued to raise questions for many hospital-employed providers, including RDNs who are delivering care via telehealth from the Hospital Outpatient Department.
Learn moreThe Academy’s work in Inclusion, Diversity, Equity and Access focuses on continued and expanded IDEA consideration at every level — cultivating organizational and professional values of equity, respect, civility and anti-discrimination.
Learn more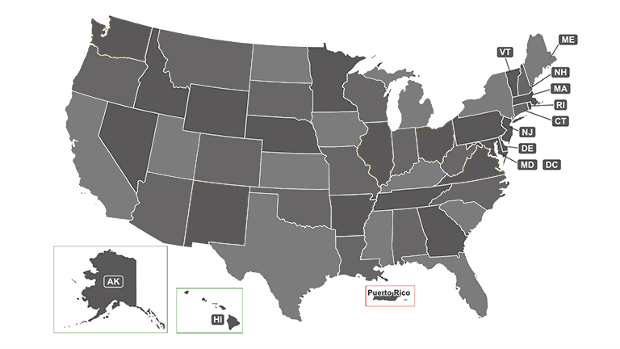
Improvements reflect a new, more judicious approach to the map to ensure members have the information necessary to practice lawfully. Learn more and see how it works.
Learn more
The Academy of Nutrition and Dietetics has created two new resources as exclusive member benefits to help practitioners succeed in their practice: the MNTWorks Toolkit and the Power of Payment series.
Learn moreSix Academy members and credentialed practitioners were selected to serve on the 2025-2030 Dietary Guidelines Advisory Committee, which is comprised of 20 members who are highly qualified nutrition scientists with demonstrated expertise.
Learn more
The Academy makes commitment to support White House Conference on Hunger, Nutrition and Health goal of ending hunger and increase healthful eating and physical activity by 2030.
Learn more
RDNs, NDTRs and other Academy members who work in pediatric nutrition, community and public health and in other settings have been actively engaged in mitigating the impact of the infant formula shortages on nutrition security for clients and patients.
Learn more
The Academy has submitted the names of 25 member experts as nominees to serve on the 2025-2030 Dietary Guidelines Advisory Committee.
Learn moreThe Academy has transitioned Food & Nutrition Magazine® content — including feature articles, practice trends, research briefs and app reviews — to a new home on eatright.org and eatrightPRO.org.
Learn moreThe Academy is seeking nominees for the 2025-2030 Dietary Guidelines Advisory Committee, which conducts rigorous analysis of research questions and is comprised of highly qualified nutrition scientists with demonstrated expertise.
Learn moreMember profiles in the MyAcademy area of eatrightPRO now have expanded gender options.
Learn moreThe National Clinical Care Commission has released "Report to Congress on Leveraging Federal Programs to Prevent and Control Diabetes and Its Complication."
Learn moreThe Academy facilitates external quality measures and standards collaborations with members.
Learn moreTwo Academy member awards have been renamed to recognize and honor the accomplishments of the award recipients.
Learn more12/29/2020 - The Academy is conducting a thorough review of the 2020-2025 Dietary Guidelines for Americans released on December 29 by the U.S. Department of Health and Human Services and the U.S. Department of Agriculture.
Learn moreDiversity and Inclusion Committee is working with numerous Academy groups and organizational units on the holistic implementation of diversity and inclusion efforts throughout the organization.
Learn more08/14/2020 - The 2020-2025 Dietary Guidelines for Americans must be informed by rigorous, scientific evidence that represents all Americans. Thanks to the input received by members, yesterday, the Academy submitted its recommendations for the Dietary Guidelines Advisory Committee's Scientific Report.
Learn moreMembers of the Academy of Nutrition and Dietetics receive exciting benefits including complimentary continuing professional education opportunities, discounts on events and products in eatrightSTORE.org, invitations to exclusive members-only events and more!
