Quality Measures
The Centers for Medicare and Medicaid Services (CMS) collects and analyzes information to produce reports utilizing quality improvement and quality measurement data. These reports are then used to improve outcomes while reducing burden on clinicians and providers.
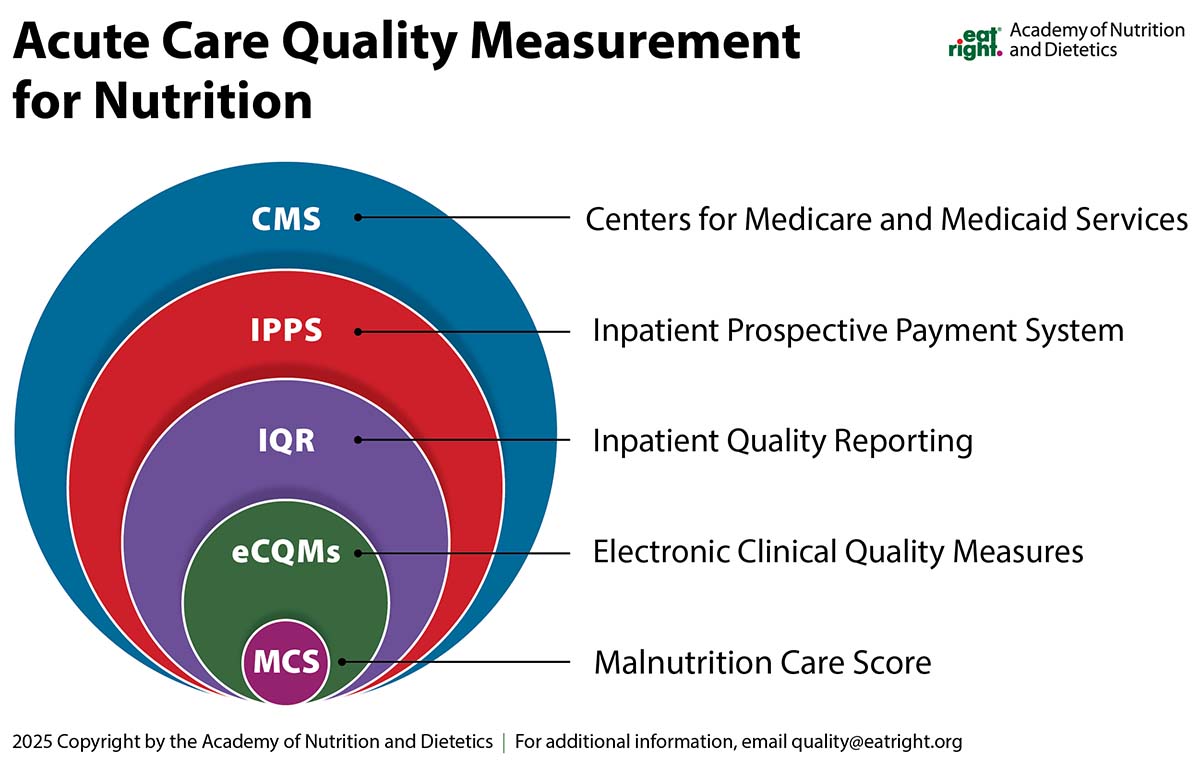
Within the CMS programs lies the Inpatient Quality Reporting (IQR) Program, a pay-for-reporting initiative that requires hospitals to submit quality and safety data to reduce complications, lower mortality rates, and deliver high-quality care. These results are publicly shared on the Care Compare website.
Electronic clinical quality measures (eCQMs), part of the IQR Program, leverage data extracted from electronic health records (EHR) or health information technology (HIT) systems to assess care quality. Hospitals submit eCQM data directly from these systems.
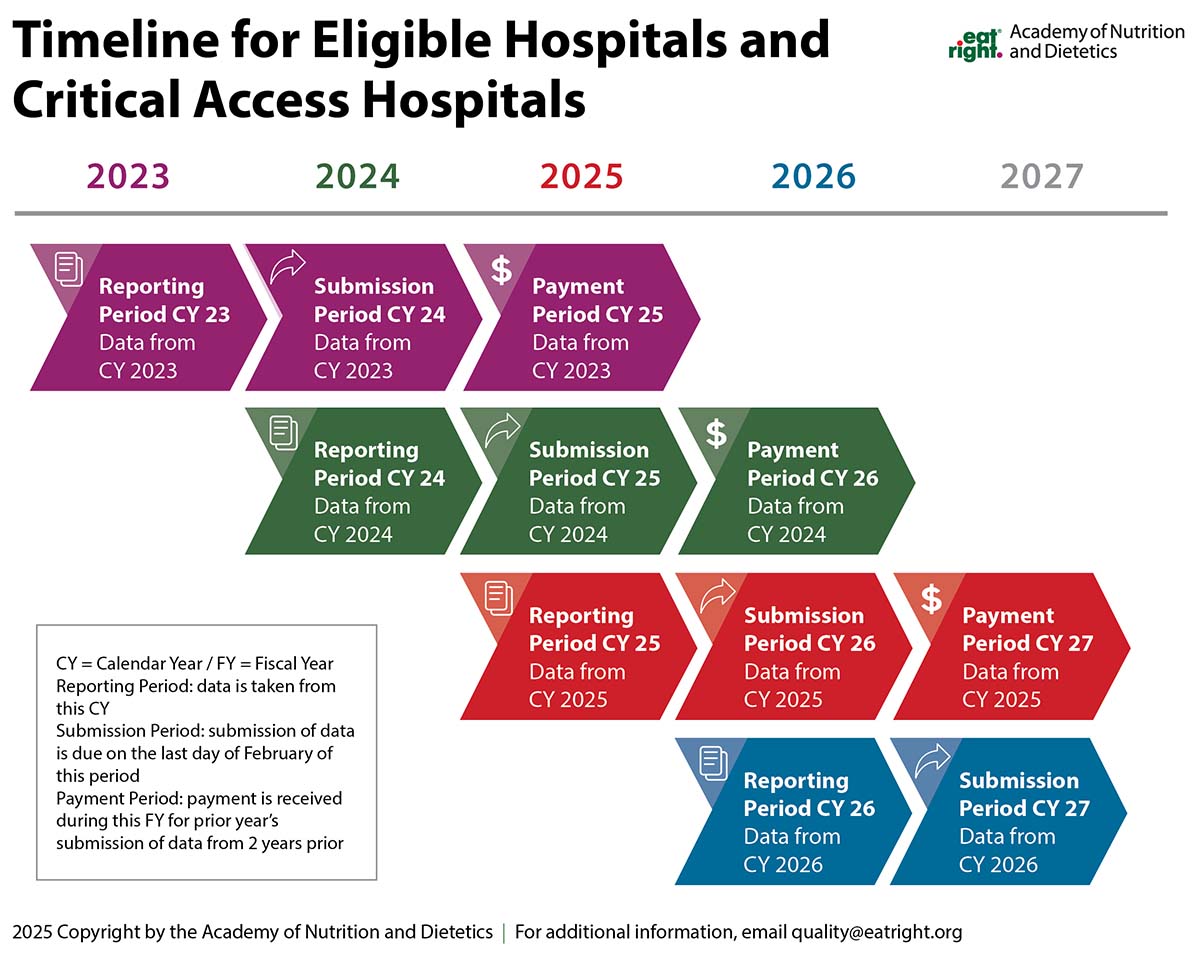
For Reporting Period 2024-2025, Eligible Hospitals and Critical Access Hospitals must report on six electronic clinical quality measures for each reporting period-three mandatory and three self-selected. The MCS was approved as a self-selected eCQM and is one of 11 eCQMs available for reporting period 2026 and beyond.
When implementing the MCS, understanding key reporting terms is crucial. The Reporting Period is the calendar year that the data will be collected. The data collected will then be submitted the following year, during the Submission Period. Ultimately, the data reported and submitted will directly be linked to the Payment Period Fiscal year that corresponds to the year after the Submission Period.
References
Join the Academy
Members of the Academy of Nutrition and Dietetics receive exciting benefits including complimentary continuing professional education opportunities, discounts on events and products in eatrightSTORE.org, invitations to exclusive members-only events and more!
