
Summary of Science: Diagnosing Pediatric Malnutrition for the Practicing Clinician
The ideal process to identify malnutrition is two-fold: nutrition screening followed by nutrition assessment.
Learn moreThe Academy's offices will be closed from December 24 through January 4, 2026, reopening on January 5. During this time, the eatrightPRO.org website will be available 24/7 to help meet your needs.
Discover the latest trends and advancements in nutrition and dietetics with insights into their impact on patient outcomes and dietetics practice. Stay up-to-date on hot topics in the field, gain valuable knowledge on consumer trends and explore the potential effects of emerging research in nutrition. Enhance your understanding of the evolving landscape of nutrition and dietetics for better-informed decision-making.

The ideal process to identify malnutrition is two-fold: nutrition screening followed by nutrition assessment.
Learn more
While healthy eating patterns can reduce the risk of many health conditions, access to nutritious foods remains a barrier for many Americans. Food as Medicine initiatives work to remove these barriers.
Learn more
Sometimes known as liquid gold, nutrient-dense colostrum is the first milk individuals who breastfeed produce before their mature milk supply comes in. However, it’s important to note the colostrum supplements currently gaining popularity are not intended for infants.
Learn more
Soy seems to have an equal number of fans and enemies. Should we go out of our way to eat more soy or avoid it? Unlike some hot-button food trends, there is a lot of research on soy, allowing food and nutrition professionals to offer evidence-based answers to questions and concerns about soy-based foods and beverages.
Learn more
Considered one of the most contagious infectious diseases, the release of a measles vaccine in 1963 led to significantly fewer cases in the United States. However, recent outbreaks have raised the question of if there are nutrition interventions that can be used to treat or prevent it.
Learn more
Serving as an expert witness is not mandatory and, if contacted by an attorney, an individual may decline. However, there are several reasons someone may choose to serve as an expert witness.
Learn more
Nova is the name for the system developed by the Center for Epidemiological Studies in Health and Nutrition, School of Public Health at the University of São Paulo in Brazil. The Nova system has four groups of processed foods, with group 1 being the least processed and group 4 being the most processed.
Learn more
On April 24, 2024, the U.S. Department of Agriculture's Food and Nutrition Services published a final rule on child nutrition programs which aligns more closely with the 2020-2025 Dietary Guidelines for Americans and will go into effect on July 1, 2024. These updates include limitations on added sugars and sodium in school meals.
Learn more
Any cancer that starts in the colon or rectum is considered colorectal cancer. Colorectal cancer is currently the fourth leading cause of cancer and the second highest cancer-related cause of death in the U.S., based on 2023 estimates.
Learn more
Nutrition may be an important modifiable risk factor in the strategy to prevent or delay the onset of dementia and other forms of cognitive decline. Learn about the MIND diet and its potential health benefits.
Learn more
According to data collected in 2021 by the CDC, almost 6% of children in the U.S. have been diagnosed with a food allergy, and the percentage increases with age. Although concerns still exist regarding the incidence of food allergies being on the rise, more promising research has been published in recent years focusing on their prevention.
Learn more
Interest in the glycemic index has increased over the years, as has the number of claims regarding its effectiveness, yet research evaluating its potential role in the prevention or treatment of certain health conditions is still evolving. Learn more, including how RDNs can translate the science when speaking to patients or clients.
Learn more
Lung cancer is the third most common cancer in the country and has been the leading cause of cancer-related death worldwide. This article details the different types of lung cancer, risk factors, dietary strategies and the role of registered dietitian nutritionists in treatment as part of the health care team.
Learn more
If you publicly post about products or recommend services on your blog, podcast or social media platform, make sure you are familiar with — and are following — the rules of engagement.
Learn more
Detected within the last two decades, Alpha-gal Syndrome is a series of allergic reactions to the Alpha-gal carbohydrate present in non-primate mammalian meat and derivative products, such as dairy, gelatin and collagen. Learn more about this condition, which is believed to be transmitted to humans by ticks.
Learn more
Food waste and food loss are global problems that affect the future and well-being of the environment and all people. While the problem is substantial, there is a lot we can do to help solve it.
Learn more
Many factors have been associated with increased risk of developing gout, including age, sex, genetics, medical conditions, overweight and obesity, severe illness or surgery, certain medications, and alcohol consumption. Although particular foods and dietary patterns have been shown to elevate serum levels of uric acid, recent research suggests genetics may play a more influential role in explaining variances in serum urate levels.
Learn more
While the Female Athlete Triad may be better known among health professionals, energy deficiency among athletes is not unique to females. There is now an evidence base to support a comparable syndrome in males, and both conditions are distinct from Relative Energy Deficiency in Sports (RED-S).
Learn more
Current evidence does not support a single ideal eating pattern for everyone with diabetes; the key to achieving optimal health and nutrition is individualization. Learn more including the RDN's role in providing medical nutrition therapy for patients or clients with diabetes or prediabetes.
Learn more
Acne vulgaris is a complex but common skin disease that affects individuals of all ages and sexes, although, it historically has a higher prevalence among both adolescents and females. Delve into research investigating a potential link between diet and acne.
Learn more
As a less invasive treatment for weight loss, compared to other bariatric procedures, endoscopic bariatric therapies have continued to gain acceptance, especially for patients with obesity who are unable to lose weight or maintain it solely through lifestyle interventions or other methods. Learn how RDNs can support patients undergoing EBT.
Learn more
Psoriasis — a chronic inflammatory disease that affects the skin — may be impacted by certain health and nutrition considerations. Insights from recent studies help unlock the link between diet and improved psoriasis symptoms.
Learn more
Nickel is regarded as one of the most common causes of allergic contact dermatitis, an intensely itchy rash in response to prolonged and repeated contact with nickel in individuals who have a sensitivity to it. While recommendations for adults with nickel allergy may include managing symptoms by foregoing high-nickel food sources, a low-nickel diet is not currently recommended for children.
Learn more
Many of the resting metabolic rate, also known as RMR, equations that are used today by registered dietitian nutritionists are based on actual body weight. Learn about research evaluating the use of adjusted body weight and what to do if RMR can't be measured by indirect calorimetry.
Learn more
Eating a variety of foods is encouraged as a way to limit exposure to contaminants, such as arsenic. Registered dietitian nutritionists can assist parents in determining safer food choices for infants and young children and when counseling other at-risk populations.
Learn more
Parkinson's disease is a progressive, disabling, neurodegenerative disease affecting approximately 1% to 2% of the population that is over 60 years of age. Learn about the main treatments for managing this disease, nutrition considerations and more.
Learn more
There has been an increased focus on exploring the role of certain foods and diets in taming inflammation — even though a specific anti-inflammatory diet has yet to be defined.
Learn more
The use of dietary supplements in the United States has continued to rise despite concerns regarding their safety and effectiveness. A study featured in the Journal of the Academy of Nutrition and Dietetics found that adults were "two and a half times more likely" to use dietary supplements while taking prescription medication compared to adults without a diagnosed medical condition.
Learn moreIn the pediatric population, both age and sex are important considerations since body composition changes as children grow and can differ depending on their sex and maturity. In the year 2000, the Centers for Disease Control and Prevention published revised growth charts for "assessing the size and growth patterns of infants, children and adolescents" in the United States.
Learn more
Early in 2023, a Consensus Study Report on the Dietary Reference Intakes for Energy was released by the National Academies of Sciences, Engineering and Medicine.
Learn more
It is estimated that around 1 million Americans have a sesame allergy. Yet, until recently, sesame was not considered to be one of the major food allergens in the United States; labeling of sesame as an allergen on packaged food products was not required until 2023.
Learn more
Learn about this newly defined eating disorder—how it presents, factors for diagnosis, similarities to and differences from other EDs, and considerations of Scope of Practice and Standards of Professional Practice.
Learn more
Should my clients increase their fluid intake to compensate for the diuretic effect of caffeine?
Learn more
Research suggests that consuming seafood that is high in omega-3 fatty acids during pregnancy may result in "better cognitive development and language and communication development in children"
Learn more
Lead exposure continues to be an environmental health problem for millions of households in the United States.
Learn more
It is well known that sources of calcium and vitamin D are important, but there are other nutrients that can also influence bone health.
Learn more
Vinegar, specifically apple cider vinegar, has been the focus of a variety of health claims over the centuries.
Learn more
There are many types of salt available on the market, today, ranging in size, color, and even vary in terms of taste.
Learn more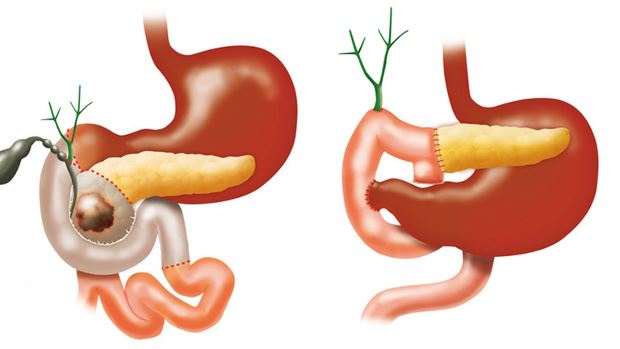
Nutritional complications that may develop from the Whipple procedure include delayed gastric emptying (gastroparesis), dumping syndrome, weight loss, diabetes mellitus, malabsorption, and nutrient deficiencies.
Learn more
About thirty-five percent of American adults develop diverticulosis by age 50 years and fifty-eight percent of adults over 60 years.
Learn more
At present, there are no validated tools to assess body mass index (BMI) in individuals with an amputation.
Learn more
A number of evidence-based resources have been published highlighting the positive outcomes associated with medical nutrition therapy encounters for patients and clients who have or are at risk for diabetes.
Learn more
Epidemiological and observational studies have shown that BMI provides an approximation of total body fat for most individuals, and it is used to define different weight groups in terms of risk for obesity-related conditions.
Learn more
One of the biggest nutritional concerns associated with achondroplasia is the predisposition to carry excess body weight, which can aggravate skeletal disorders.
Learn more
In order to differentiate between preexisting diabetes and gestational diabetes mellitus, it is recommended that women with risk factors for diabetes be tested at their first prenatal visit in their first trimester.
Learn more
Reasons for using a hemoglobin A1c test have included it being a faster and easier diagnostic test, and there is no need for fasting beforehand.
Learn more
People living with human immunodeficiency virus (HIV) or acquired immunodeficiency syndrome (AIDS) are susceptible to metabolic changes and chronic inflammation.
Learn more
After its use decreased in recent decades due to its high saturated fatty acid content, coconut oil has been making a comeback.
Learn more
There is emerging evidence that conversion of dietary nitrate and nitrite to nitric oxide may have beneficial effects in cardiovascular disease.
Learn more
The recommendations relating to the Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline have recently undergone their third revision by the European Pressure Ulcer Advisory Panel (EPUAP), the National Pressure Injury Advisory Panel (NPIAP), and the Pan Pacific Pressure Injury Alliance (PPPIA).
Learn more
There is little benefit in deliberately provoking or dividing your community. Engaging in offensive or polarizing social media behavior can lead to significant losses, such as professional reputation and potential opportunities down the line. Nevertheless, we all make mistakes, and breaching the boundaries of online etiquette doesn't have to be an irreversible act.
Learn more
In folklore, trolls live under bridges and taunt passersby. Today, trolls are no less vile. Like everything else, however, they’ve gone digital, lurking online. Their goal isn’t engaging online communities; it’s enraging them. Here are some tips to manage trolls on online forums.
Learn more
Whether you are a student, newly minted RDN or NDTR or a seasoned pro, social media and online comments can have unintended consequences on your career. Check your digital footprint to avoid losing a future job or other opportunity (without even knowing it).
Learn more
Social media platforms provide opportunities to engage and lend a global platform for civil discourse and dialogue. Unfortunately, there also are those who exploit this opportunity in order to stir the pot and seek attention. Here are some tactics for dealing with negativity online.
Learn more
Hydroponically grown lettuce, tomatoes, strawberries and herbs make up an ever-increasing share of produce on display at many grocery stores and farmers markets. But growing plants indoors in controlled conditions is hardly new.
Learn more
As vitamin K research has evolved over the years, it has led to the discovery of vitamin K-dependent reactions beyond coagulation, including proteins involved in bone metabolism.
Learn more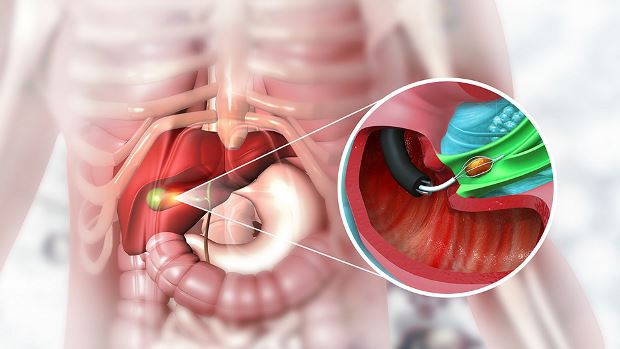
There is not a universal standard diet post-cholecystectomy and several diet modifications may be indicated.
Learn more
Eating for reasons other than hunger is a nutrition and health-related behavior that many registered dietitian nutritionists encounter when working with patients and clients.
Learn moreThe medical management of kidney stones involves a metabolic evaluation, including a 24-hour urine collection.
Learn moreIn 2019, a task force commissioned by the American College of Cardiology (ACC) and the American Heart Association (AHA) released clinical practice guidelines for the primary prevention of atherosclerotic cardiovascular disease (ASCVD).
Learn moreEach person's level of tolerance to histamine is unique and ever changing, so the approach to reduce dietary sources of histamine needs to be individualized for patients or clients with a suspected intolerance.
Learn moreMacular degeneration, also known as age-related macular degeneration (AMD), is one of the main reasons for vision loss in older adults and is the most common cause of legal blindness in the U.S. and other developed countries.
Learn moreIn recent years, the nutritional value of seed oils — often referred to as vegetable oils — has come under increased scrutiny. This brief report summarizes current evidence on the effects of seed oils on health outcomes.
Learn moreRheumatoid arthritis (RA) is a chronic inflammatory autoimmune disease that affects more than 1.5 million people in the United States.
Learn moreRDNs can assist patients with food allergies by creating strategies to avoid allergens while focusing on the nutritional adequacy overall with label reading, safe and nutritious food substitution, dining out in restaurants, managing allergens in schools and preventing cross-contamination at home.
Learn moreIn addition to concerns regarding possible hidden or harmful ingredients which may be found in dietary supplements, claims that are made in the marketing of many of these over-the-counter products can be problematic.
Learn moreIn addition to iron-related issues, patients with thalassemia are at risk for other morbidities due to poor nutritional status, and these can affect growth, bone mineralization and immune function.
Learn moreSynthetic food dyes are often used in processed foods to add and enhance color and visual appeal. While concerns surrounding the use of these additives are not new, recent advocacy efforts have renewed public interest in calling for the removal of synthetic food dyes.
Learn moreUltra-processed foods (UPFs) have emerged as a growing focus in nutrition science due to increasing evidence that these foods contribute to multiple chronic diseases. Consumption of UPFs has increased significantly, with UPFs contributing over 50% of total calorie intake in the United States, prompting concern from public health experts, dietitians and clinicians alike.
Learn moreThe pH level of food and its impact on acid-base balance plays an important role in several areas of nutrition, including food safety and medical nutrition therapy.
Learn moreThe term "Mediterranean diet" can be used to describe the eating pattern of at least 16 countries that border the Mediterranean Sea, which presents some difficulty in characterizing a Mediterranean diet.
Learn moreAccording to the Centers for Disease Control and Prevention (CDC), “Down syndrome remains the most common chromosomal condition diagnosed in the United States.”
Learn more
While it is evident that some varieties of mushrooms could be regarded as good sources of vitamin D, not all types will meet these criteria.
Learn moreThe family of compounds called salicylates is found naturally in many plants, but the amount can vary depending on the plant species and its growing conditions.
Learn moreDietary fiber is undoubtedly an essential part of a healthy eating plan, yet its effect as a nutrient has been somewhat elusive.
Learn moreRegistered dietitian nutritionists will likely encounter patients seeking nutrition counseling for suspected or diagnosed food allergies including requests such as a "yeast allergy diet."
Learn moreA regular question received by registered dietitian nutritionists in the United States focuses on how much weight is gained on average during the holiday season.
Learn moreAlthough many complications related to obesity can resolve following weight loss surgery, there is an increased risk for nutritional deficiencies, which can influence the outcome of a healthy pregnancy.
Learn moreThe ratio of weight to height is measured in body mass index (BMI) and is used to estimate adiposity, however it does not provide information on the distribution of body fat or a full picture on individual health risks.
Learn morePKU occurs when the body is deficient in the enzyme, phenylalanine hydroxylase, which converts the essential amino acid phenylalanine (Phe) to tyrosine.
Learn moreMembers of the Academy of Nutrition and Dietetics receive exciting benefits including complimentary continuing professional education opportunities, discounts on events and products in eatrightSTORE.org, invitations to exclusive members-only events and more!
